Myth: The Modified Barium Swallow is the ‘Gold Standard’ in swallowing diagnostics because it has been around for more than 50 years in treatment of swallowing disorders.
Reality:
Reality:
- The multidisciplinary study of swallowing and swallowing disorders has evolved over the past thirty years.
- Prior to 1976, various types of dysphagia were recognized but largely left untreated. The coordinated assessment and, more importantly, treatment of patients with swallowing disorders did not begin in the late 1970s. (Evan B Page, MA CCC-SLP, Radiographic Imaging LLC, “Understanding the MBS History”)
- MBS became a standard tool for diagnosing dysphagia in the early 1980’s.
Myth: Using Fiberoptic Endoscopy for swallowing instrumentation is a new idea.
Reality:
Reality:
- The first endoscopy studies for swallowing disorders occurred just a few years after the initiation of the MBS as a tool for swallowing diagnostics.
- In 1984, the first articles on evaluating swallowing disorders with endoscopy began circulating in the healthcare community.
- By the late 80’s, FEES, or fiberoptic endoscopic evaluation of swallowing was being studied in several VA and Teaching Hospitals across the country.
- In 1992 FEES became an official part of the ASHA scope of practice for Speech Pathologists with additional training to perform the evaluation.
Myth: The MBS is the preferred instrumentation. It’s easy on the patient with no side effects.
Reality:
Reality:
- The MBS study is performed in a radiology suite and requires cooperation on the part of the patient.
- Aspiration of Barium Sulfate can be very dangerous to the respiratory-compromised patient. (Acute pneumonitis caused by low-density barium sulphate aspiration. (J. P. M. Pracy a1 c1, P. Q. Montgomery a1 and N. Reading a1 a1 (London))
- Barium can remain in the colon for 6 weeks or longer in the elderly patient, causing severe constipation or complications from intestinal blockage. (Morcos 2000)
- Cognitively compromised patients can become very frightened by the experience.
Myth: I can see aspiration on an MBS but not with endoscopy.
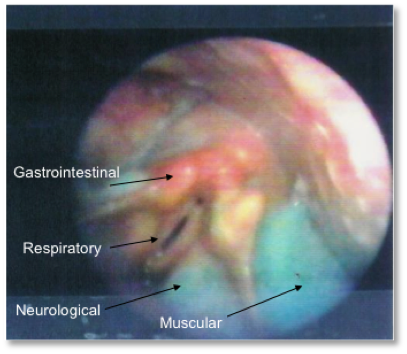
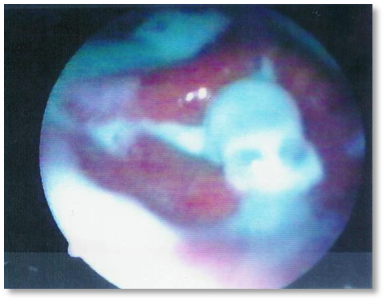
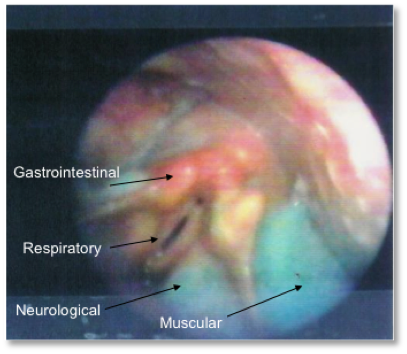
Reality: Aspiration is clearly visible with endoscopy (right):
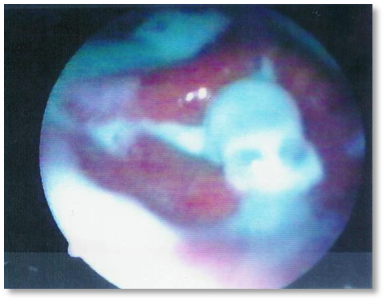
Reality: Aspiration is clearly visible with endoscopy (right):
Myth: I can see everything I need to see on an MBS.
Reality: Secretions are invisible on MBS (left) but not with endoscopy (right):


Reality: Secretions are invisible on MBS (left) but not with endoscopy (right):


Myth: I need to see the esophageal stage of the swallow with the MBS to treat effectively.
Reality: Reflux or G-Tube feeding invisible on the MBS (left) and visible on endoscopy (right):

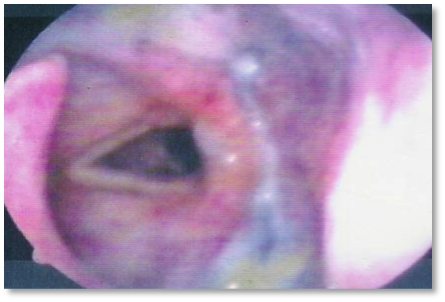
Reality: Reflux or G-Tube feeding invisible on the MBS (left) and visible on endoscopy (right):

Myth: Passing the endoscope hurts and is traumatic to the patient.
Reality:
Reality:
- In a 1,000 consecutive patient study, the average change in BP/Pulse was less than 0.3.
- There has never been a reported “adverse reaction” to endoscopy in the 23+ years that this team has been providing services.
- A properly trained SLP endoscopist performs the test virtually pain-free.
- The DMS SLP is trained for all patient types, including dementia patients.
Myth: The endoscope goes “up the nose.”
Reality: The endoscope is passed along the floor of the nose, straight back to the hypo-pharynx. The ‘spaghetti-sized’ endoscope then looks down into the pharynx to view the swallow.
Reality: The endoscope is passed along the floor of the nose, straight back to the hypo-pharynx. The ‘spaghetti-sized’ endoscope then looks down into the pharynx to view the swallow.
Myth: I need to know the quantitative amount of aspirate for each aspirated consistency in order to treat effectively.
Reality: It is never just one consistency or one swallow, but rather a combination of issues that results in complications from dysphagia.
Reality: It is never just one consistency or one swallow, but rather a combination of issues that results in complications from dysphagia.